What Causes High Eye Pressure and How to Reduce It?
July 30, 2024
Have Any Questions?
Please contact us, if you have any queries
Categories

Many eye-related concerns and fatal conditions, like glaucoma, can be caused by increased intraocular pressure, commonly known as higher pressure inside the eye. A permanent loss of eyesight and serious visual difficulties may result from this elevated pressure, which can also harm the optic nerve. Maintaining ocular pressure within the normal range becomes crucial, considering this. The reasons, signs, and treatments for elevated intraocular pressure will all be covered in this piece. Maintaining proper eye health and maintenance can be greatly aided by having learned these facts.
What is High Eye Pressure?
Medical terminology refers to high eye pressure, or ocular hypertension, as a condition when the intraocular pressure, or pressure inside the eye, rises above normal. Considering the range, the typical eye pressure is considered within the range of 10 mm Hg and 21 mm Hg. If your ophthalmologist finds that the eye pressure has surpassed this range, they may suggest a few more tests and start high eye pressure treatment.
Although eye pressure cannot be regarded as an illness in itself, it may be a sign of an underlying condition such as glaucoma. As elevated eye pressure can eventually cause damage to the optic nerve and severe visual impairment, it is crucial to detect it and treat it as soon as possible.
Causes of High Eye Pressure
Knowing what elevated ocular pressure means, it is imperative to ascertain the reason for an increase in ocular pressure above normal. The following are the most typical reasons for excessive ocular pressure:
- Overproduction of Aqueous: The excessive production of aqueous humor, or the fluid in the eye, is one of the primary causes of high intraocular pressure. Aqueous humor can build up and exert more pressure inside the eye when it is produced at a pace that exceeds its drainage.
- Slow Aqueous Drainage: An additional factor leading to the buildup of aqueous humor in the eye is a malfunctioning drainage mechanism.
- Eye Trauma: Eye trauma can result in an imbalance between the aqueous humor’s production and drainage, which raises the pressure inside the eyes.
- Medication: Some drugs, especially steroids and steroidal eye drops, can potentially raise the intraocular pressure.
- Other Eye Conditions: Pigment Dispersion Syndrome and corneal arcus are examples of conditions that are also associated with increased eye pressure.
Symptoms
The following are some of the common symptoms of elevated intraocular pressure:
- Pain in and around the eyes- A throbbing or soreness, particularly while moving.
- Blurred vision- Impairment of clear vision.
- Blind areas- The visual field contains blind areas.
- Red eyes- Irritability and redness
- Eye Soreness- Sensitivity and pain.
- Headaches- headaches that never go away.
Your ophthalmologist may run certain tests to measure your intraocular pressure in order to determine the best course of action if you experience any or all of the aforementioned symptoms.
Treatment of High Eye Pressure
Both medication and surgery are methods employed to manage excessive ocular pressure. Primarily, your ophthalmologist will use pharmaceutical eye drops to lower intraocular pressure. If medication and eye drops fail to reduce the elevated pressure, your ophthalmologist might recommend surgery as a treatment option.
Medications
- Topical medications: The first phase of treatment is typically eye drops that either decrease the amount of fluid produced in the eye or enhance its evacuation.
- Oral Medications: If eye drops fail to work, a prescription for an oral drug may be given.
Lifestyle Changes
- Healthy Diet: Consuming a well-balanced diet that includes plenty of zinc, copper, selenium, and the vitamins C, E, and A can help maintain eye health. Two especially healthy foods are leafy greens and omega-3 fatty acids.
- Physical activity: Physical activity on a regular basis can help lower eye pressure, but it’s crucial to stay away from exercises that strain the eyes.
- Limit Your Caffeine Intake: It’s advisable to consume caffeine in moderation, as too much of it can raise your ocular pressure.
- Stress Reduction: Eye pressure can be controlled with the help of stress-reduction methods such as yoga, meditation, and other approaches.
Advanced Treatments
- Laser therapy: This treatment could improve the eye’s ability to clear liquid.
- Surgical Procedures: In more extreme circumstances, new drainage channels might be created during surgery to release pressure.
Preventative Measures
Preventing high blood pressure and its potential negative effects demands maintaining a healthy lifestyle. The following are some preventative actions to think about:
• Routine eye exams: Consulting your ophthalmologist on a regular basis might help identify changes in eye pressure early on.
• Protective eyewear: Using protective eyewear might help avoid trauma-induced pressure rise when engaging in activities that could injure the eyes.
• Keep an Eye on Your Health: Controlling long-term health issues like diabetes and high blood pressure can also help lower eye pressure.
• Good Habits: Reducing alcohol intake and smoking can help maintain general eye health.
Potential Consequences of High Eye Pressure
If left untreated, high ocular pressure can result in a number of complications. The most serious threat is developing glaucoma, which can result in vision loss and irreparable damage to the optic nerve. For the early detection and prevention of glaucoma, routine eye exams are crucial.
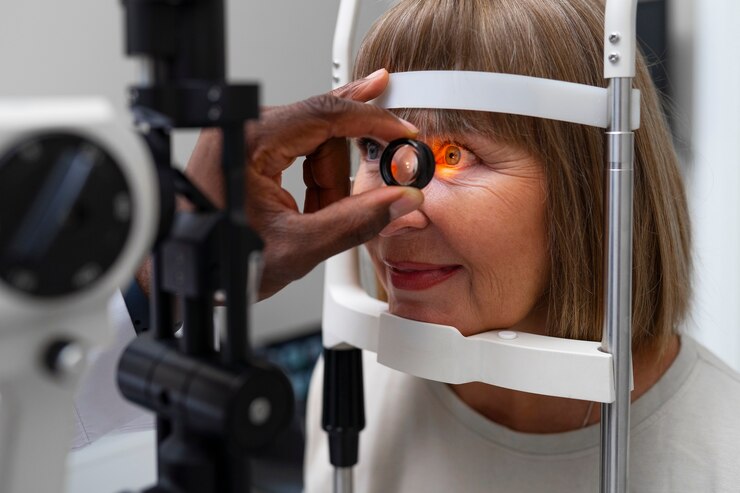
Maintaining eye health requires routine eye exams, particularly for people who are at risk of high eye pressure. In order to identify any early indicators of glaucoma or other eye disorders, an ophthalmologist can measure intraocular pressure, evaluate the optic nerve, and conduct visual field tests during an eye exam. Vision protection and the prevention of major eye illnesses can be achieved through early detection and treatment.
Reach out to RMC for all-inclusive eye care
Maintaining one’s eye health is important for overall well-being. Even though high eye pressure is frequently asymptomatic, improper management can result in catastrophic disorders like glaucoma. Effective management of high eye pressure requires consistent adherence to prescribed therapies, a healthy lifestyle, and routine eye exams. Don’t let your eye health be a chance; talk to your optometrist about your eye pressure during your next examination and take preventative measures to save your vision.
Comprehensive and preventative care is what we at RMC believe in. Make an appointment with us if you need a consultation or if you’re worried about any other concerns. Our team is committed to giving you the finest treatment possible to safeguard your health.