Through the Rain and Mist: A Gentle Guide to Monsoon Eye Wellness
The rains bring a quiet poetry to life petrichor rising from the earth, shimmering puddles on city streets, the soft hush of clouds blanketing the sky. But amid this calm and chaos, the monsoon also brings with it an undercurrent of health concerns, many of which quietly take root in places we often overlook our eyes.
With rising humidity, fluctuating temperatures, and water-borne irritants, our eyes become more vulnerable than ever during the monsoon months. While we often take precautions for colds, fevers, and skin infections, the eyes so delicate, so exposed, require a special kind of care. This season, let’s look beyond the umbrella and raincoat. Let’s shield our vision.
Why Eyes Are at Risk During Monsoons
The monsoon may feel like a respite after scorching summer days, but this seasonal shift fosters an environment perfect for bacterial and viral growth. Waterlogging, unclean hands, contaminated rainwater, and excessive rubbing can cause eye infections that range from mild irritations to serious conditions like conjunctivitis, styes, and keratitis.
Humidity, while pleasant in small doses, also tends to trap allergens in the air, aggravating pre-existing issues such as dry eye syndrome or allergic conjunctivitis.
Signs You Shouldn’t Ignore
During this season, our eyes often try to tell us when something is amiss. Recognizing the signs early can help prevent escalation. Look out for:
- Persistent redness
- Excessive watering or discharge
- Itchiness or burning sensation
- Blurry or double vision
- Swelling around the eyes or eyelids
- Sensitivity to light
Any of these symptoms should prompt immediate consultation with an eye specialist. Delay can not only increase discomfort but also risk more serious infections.
Your Monsoon Eye Care Companion: Practical, Gentle Tips
To ensure that the rains don’t cloud your vision literally or figuratively here are some elegant yet effective monsoon eye care tips that you can integrate effortlessly into your daily routine.
- Hands Off the Eyes
This simple yet critical rule cannot be repeated enough. Rainy weather can make hands more prone to contamination. Avoid touching or rubbing your eyes, especially when you’re outdoors. Carry a personal hand sanitizer and use it before adjusting contact lenses or touching your face.
- Use Clean, Filtered Water to Rinse
If you feel irritation or a foreign body sensation in the eyes, avoid splashing with regular tap water, especially during the monsoon. Use clean, filtered, or boiled water to rinse your eyes. Even better—consult your ophthalmologist before attempting self-cleaning.
- Keep Your Eye Makeup Minimal (or Sterile)
For those who use makeup, monsoon isn’t the time to experiment with kajals or liners that may smudge and introduce bacteria. Always remove makeup before sleeping and avoid sharing cosmetics. Discard any eye products that have crossed their expiration date, and never use makeup during an eye infection.
- Protective Eyewear—Not Just a Summer Affair
Most people think of sunglasses as a summer staple, but wearing protective glasses during the monsoon can shield your eyes from dust, rainwater, and allergens. Choose glasses with an anti-reflective coating if you’re often driving in the rain or walking on busy roads.
- Say No to Rainwater in the Eyes
That first shower may feel like a blessing, but rainwater, especially in urban areas, is often acidic and contaminated with pollutants. Avoid letting rainwater enter your eyes, and if it does, rinse gently with clean water and pat dry with a soft, sterile cloth.
- Switch to Daily Disposable Lenses (If You Can)
Contact lens wearers are particularly vulnerable to infections during this season. If possible, switch to daily disposable lenses to reduce the risk of bacterial buildup. Ensure you wash and dry your hands thoroughly before inserting or removing lenses. And always, always avoid sleeping in them.
- Keep Towels Personal and Dry
Avoid sharing handkerchiefs or towels—even with family members. Ensure your face towel is soft, clean, and completely dry before using. Damp towels can be a breeding ground for bacteria and fungi.
- Avoid Self-Medication, Especially Eye Drops
Not all eye drops are created equal. What works for redness may worsen an infection. Avoid reaching for over-the-counter drops without medical guidance. Prolonged or incorrect use of steroid-based drops, for example, can aggravate underlying conditions.
- Eat for Your Eyes
Yes, nutrition matters. Include foods rich in Vitamin A, omega-3 fatty acids, and antioxidants in your monsoon diet. Leafy greens, citrus fruits, carrots, and nuts like almonds can help keep your eyes healthy from the inside out.
- Don’t Ignore Screen Hygiene
Rainy days often lead to more indoor time—and more screen time. Maintain a proper viewing distance, follow the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds), and ensure your screens are free of glare and well-lit.
- Visit Your Eye Specialist, Rain or Shine
Make it a habit to get regular eye checkups, especially if you’re prone to allergies or already wear spectacles or lenses. Many infections can be prevented with early diagnosis and simple interventions.
Special Care for Children and the Elderly
Children often play in puddles or get drenched in the rain, and may not communicate eye discomfort well. The elderly, on the other hand, may ignore subtle signs of infection or vision changes, assuming them to be “just age.” For both these age groups, gentle monitoring is key.
If your child comes home after the rain, check for redness or itchiness. For elders, keep an eye on symptoms such as blurred vision, eye pain, or discharge.
Rain-Proofing Your Eye Habits
- Carry a soft, dry tissue or sterile eye wipes when stepping outdoors.
- Invest in an umbrella that provides full face cover.
- Avoid crowded or dusty places when possible.
- Take small breaks from air-conditioned environments, which can dry out the eyes.
- Keep a spare pair of spectacles in your bag, especially if you wear lenses.
When the Clouds Settle…
The monsoon is more than just a seasonal occurrence it is a rhythm of nature, a cleansing, a quiet shift. But within this romantic deluge lies the responsibility of care. Of listening to your body. Of not mistaking a minor irritation for a passing glitch.
Your eyes, after all, do not merely see the world they reflect your well-being.
Where Expertise Meets Empathy
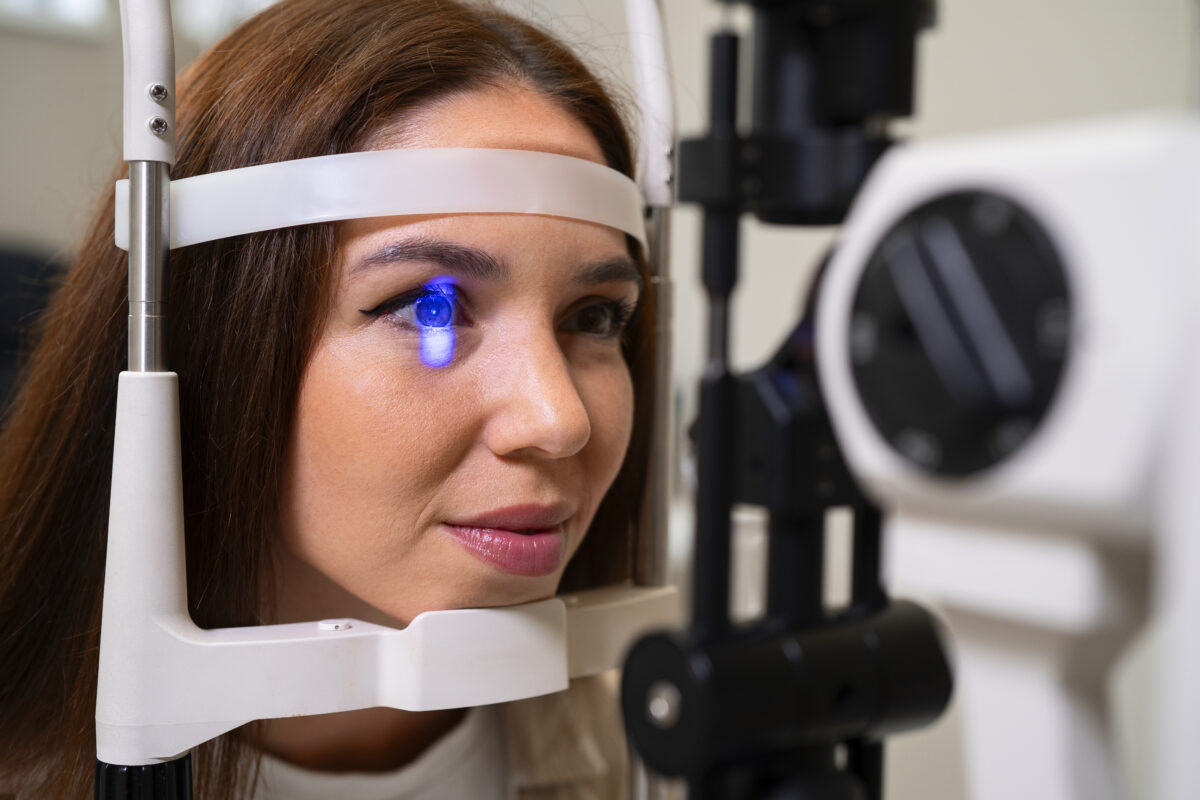
At Rani Menon Maxivision Eye Hospital, our vision for eye care is rooted in precision, compassion, and innovation. With state-of-the-art diagnostic tools and a team of seasoned ophthalmologists, we are equipped to treat all kinds of monsoon-related eye concerns from common infections to rare complications.
Whether it’s a routine check-up or a persistent irritation, our focus remains the same: your clarity, your comfort, your care. As the skies change colour, let your eye care routine evolve too. We’re here, rain or shine.
Let this monsoon not cloud your vision, but clear your path to better eye health.
For appointments or expert consultations, visit your nearest Rani Menon Maxivision Eye Hospital branch or connect with us online.