When it comes to healthcare, trust is built slowly, through years of care, compassion, and consistent excellence. In Thrissur, countless families have found that trust in one name: a dependable eye hospital in Thrissur that has been caring for generations with dedication and integrity.
From grandparents who once came in for cataract treatment to their grandchildren who now visit for regular eye check-ups, this lasting bond between families and our eye care hospital in Thrissur tells a story beyond medicine; a story of relationships, reliability, and a shared vision for lifelong eye health.
A Legacy of Trust That Spans Generations
In a world where medical choices are many, what makes families return to the same eye hospital for decades? The answer lies in the legacy of trust we’ve built.
For years, our eye hospital in Thrissur has been synonymous with quality eye care. What began as a small initiative to provide reliable treatment has now grown into a center of excellence, equipped with advanced technology and some of Kerala’s finest ophthalmologists.
But what truly keeps families coming back isn’t just the innovation, it’s the unwavering commitment to care that feels deeply personal. Every generation that steps into our hospital feels that familiar sense of comfort, knowing their eyes are in trusted hands.
- Expertise That Inspires Confidence
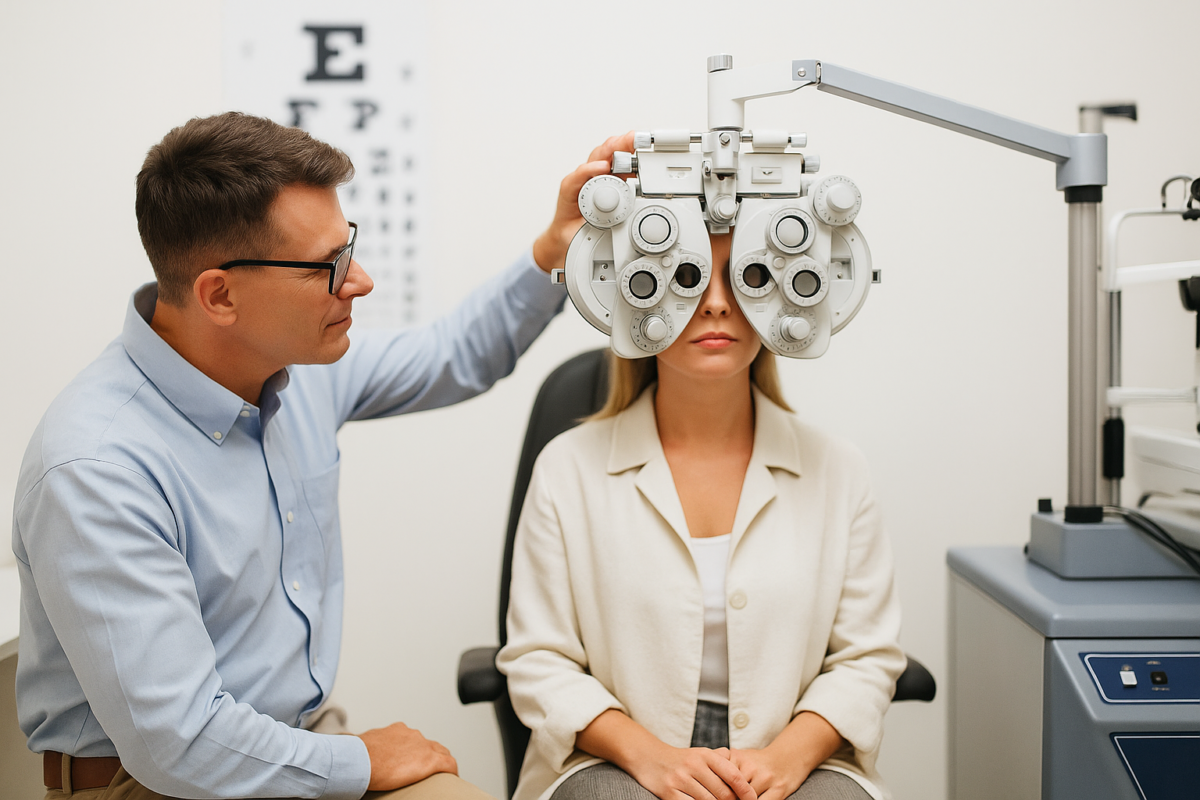
The foundation of our reputation lies in our team of highly skilled ophthalmologists and specialists. Each doctor brings not just years of experience but also a passion for precision and patient care.
Our specialists continuously update their knowledge through advanced training, ensuring that patients receive the latest, most effective treatments available. Whether it’s cataract surgery, diabetic eye care, or corneal and retinal procedures, we approach every case with expertise and compassion.
Families in Thrissur trust our eye care hospital because they know our doctors don’t just treat symptoms, they understand the person behind the condition. Every consultation begins with listening, explaining, and guiding, creating a care experience rooted in trust.
- Cutting-Edge Technology for Clearer Vision
The field of ophthalmology is ever-evolving, and we’ve always been ahead of the curve. Our eye hospital in Thrissur is equipped with advanced diagnostic and surgical tools, ensuring accurate assessments and highly successful treatment outcomes.
From precision-based cataract surgeries using premium intraocular lenses to advanced retina scanning and corneal imaging, every aspect of patient care is supported by world-class technology.
This commitment to technological excellence ensures that patients of all ages, from children to adults and seniors, receive the safest and most effective care possible. For families, it’s reassuring to know that their loved ones are being treated with the same standards found in top global eye centers.
- Compassionate, Family-Centered Care
At the heart of our hospital’s philosophy lies compassionate care. We believe that great eye care isn’t just about technology or medicine; it’s about people. We welcome every patient as if they were a member of our own family.
Our staff goes beyond routine procedures to ensure comfort, clarity, and confidence at every stage of treatment. Whether it’s helping a nervous child before an eye test or reassuring an elderly patient before surgery, we make sure every experience is warm, calm, and reassuring.
This empathetic approach has made us more than just a leading eye care hospital in Thrissur; we’ve become a trusted part of countless family stories. Parents recommend us to their children, siblings bring each other for checkups, and entire households rely on our expertise to protect their vision.
- Comprehensive Eye Care Under One Roof
Families trust us because they know that whatever their eye care needs are, we can handle them all under one roof. Our eye hospital in Thrissur offers a full spectrum of services, including:
- Cataract evaluation and surgery with advanced lens implants
- Retina and diabetic eye care for long-term vision protection
- Glaucoma diagnosis and management
- Pediatric and squint correction treatments
- Refractive surgeries (LASIK, SMILE, etc.) for spectacle-free vision
- Corneal treatments and dry eye management
This all-inclusive approach ensures that every member of the family receives consistent, high-quality care without needing multiple hospital visits or referrals.
- Transparent, Ethical, and Honest Practice
One of the biggest reasons families continue to choose our eye care hospital in Thrissur is our unwavering commitment to ethics. We believe that medical treatment should always be transparent, honest, and centered on the patient’s well-being.
We clearly explain every diagnosis, discuss all available options, and help patients make informed decisions, without pressure or hidden costs. This honesty has earned us something far greater than just recognition: it has earned us the long-term trust of our community.
In an era where commercial healthcare often overshadows compassion, our hospital continues to stand out for its ethical approach and patient-first philosophy.
- Generational Bonds: More Than Just Patients
Over the decades, we’ve seen something truly special: families returning with stories that go back generations. A grandfather who had his cataract removed years ago now brings his granddaughter for her first eye checkup. A mother who trusted us for her diabetic eye care recommends us to her son, who works in another city.
These are not just appointments, they’re relationships built on years of satisfaction, trust, and gratitude. Being a part of such generational stories is our greatest achievement as an eye hospital in Thrissur.
- Accessible Care with a Local Touch
While we offer treatments that meet international standards, our hospital has never lost its local touch. We understand the people of Thrissur; their needs, their expectations, and their lifestyles.
We’ve made sure our services remain affordable, accessible, and inclusive, so that no one has to compromise on quality due to cost or distance. Our friendly staff ensures smooth appointments, timely care, and personalized attention for every patient.
Families know that when they visit our eye care hospital in Thrissur, they’ll always receive genuine care from people who truly understand them.
- Commitment to Preventive and Lifelong Eye Health
Good eye care doesn’t end with a single treatment; it’s a lifelong commitment. That’s why our hospital focuses strongly on preventive eye care and regular eye check-ups.
We organize awareness programs, free eye camps, and diabetic eye screenings across Thrissur to educate people about the importance of early detection. Our goal is simple: to help every individual enjoy clear, healthy vision for life.
By staying connected with our patients even after treatment, we ensure that families remain informed, proactive, and confident about their eye health.
Why Families Continue to Choose Us
In essence, our success story is not about numbers or awards; it’s about trust, built through decades of compassionate service. Generations of families have chosen our eye hospital in Thrissur because we’ve never wavered from our founding values:
- Medical excellence rooted in compassion
- Honesty in every consultation
- Advanced treatments delivered with empathy
- Lifelong commitment to eye health
For us, every restored vision, every smile after surgery, and every “thank you” from a patient reinforces why we do what we do.
Conclusion: A Vision of Care That Lasts a Lifetime
As Thrissur continues to grow, our eye care hospital remains deeply connected to the people who have made us what we are today. We’re proud to be more than just a healthcare institution; we’re a part of countless families’ stories, protecting their sight and preserving their trust for generations.
So if you or your loved ones are looking for reliable, advanced, and compassionate eye care, look no further. Experience the warmth and expertise that generations in Thrissur have trusted, because when it comes to your vision, you deserve nothing but the best.