As the refreshing monsoon showers bring relief from the scorching summer heat, they also open the door to a variety of health issues, and your eyes are no exception. Increased humidity, stagnant water, and rising allergens in the air during the monsoon season can create the perfect breeding ground for bacteria and viruses, often resulting in eye discomfort and infections.
This blog explores why eye irritation is more common during the rainy season and what you can do to protect your eyes. Whether you’re experiencing itchiness, redness, or watery eyes, understanding the causes and prevention methods can save you from unnecessary distress. If symptoms persist, seeking eye specialist treatment in Thrissur or anywhere nearby is crucial for prompt relief.
Why Does Eye Irritation Increase During the Monsoon?
Monsoon weather creates ideal conditions for microbial growth. The combination of warm temperatures and high humidity allows bacteria, fungi, and viruses to thrive, many of which can easily spread through air, water, or contact with contaminated hands and surfaces. Here are the key reasons why eye problems surge during this season:
- Bacterial and Viral Infections
Waterborne and airborne infections are rampant during monsoon months. Conjunctivitis (commonly called “pink eye”) is one of the most frequent eye issues seen during this time. It’s highly contagious and can spread through shared towels, handshakes, or touching the eyes with unwashed hands.
- Increased Allergen Exposure
Rainfall can wash pollen and dust into the air temporarily, increasing exposure to allergens. These can trigger allergic conjunctivitis — causing red, itchy, and watery eyes. People with sensitive eyes or pre-existing allergies are especially vulnerable.
- Fungal Infections
Damp environments promote fungal growth. Eye infections such as keratitis — an inflammation of the cornea — may occur due to prolonged exposure to contaminated water or poor hygiene while handling contact lenses.
- Contact Lens Complications
People who wear contact lenses may face greater risks during the monsoon. The risk of microbial contamination increases when lenses are not cleaned properly or when rainwater enters the eyes while wearing lenses.
- Environmental Irritants
Monsoon floods can cause sewage water to mix with street water, leading to exposure to harmful irritants. Splashing into such water or rubbing the eyes after contact can lead to inflammation or serious infections.
Common Eye Problems During Monsoon
Below are some of the typical eye conditions people report during the rainy season:
- Conjunctivitis (viral or bacterial): Redness, itching, sticky discharge
- Stye: A painful lump near the edge of the eyelid caused by bacterial infection
- Dry Eyes: Surprisingly common due to indoor air conditioning or reduced blinking during screen use
- Allergic Conjunctivitis: Itchy, watery eyes triggered by allergens
- Keratitis: Redness, blurred vision, and sensitivity to light caused by corneal infection
If you notice these symptoms persisting beyond a couple of days, consult an expert for eye vision treatment in Kerala before it worsens.
Tips to Prevent Eye Irritation During the Monsoon
The good news is that most monsoon-related eye issues are preventable with simple hygiene and lifestyle practices. Here are practical steps to protect your eye health:
- Avoid Touching Your Eyes Frequently
Make a conscious effort to avoid rubbing or touching your eyes, especially with unwashed hands. This is the most common way bacteria and viruses spread.
- Use Protective Eyewear
Wearing sunglasses or clear protective glasses can shield your eyes from rainwater splashes, wind, and dust. This is especially helpful for two-wheeler riders.
- Maintain Contact Lens Hygiene
Disinfect your contact lenses regularly and avoid wearing them during rain or while swimming. Never reuse lens solution and always wash your hands before handling them.
- Do Not Share Personal Items
Avoid sharing towels, handkerchiefs, or eye makeup, especially during monsoon season. This reduces the risk of infection spread among family or co-workers.
- Limit Screen Time
With increased time indoors, screen usage tends to rise. Follow the 20-20-20 rule: every 20 minutes, look 20 feet away for 20 seconds to prevent eye strain and dryness.
- Use Clean Water to Rinse Your Eyes
If your eyes feel itchy or irritated, rinse them with clean, filtered water — never with rainwater or tap water that may be contaminated.
When Should You Visit an Eye Specialist?
While minor eye discomfort can often be managed at home, there are times when professional help becomes necessary. You should consult an eye specialist for treatment in Thrissur or nearby if you experience any of the following:
- Eye redness lasting more than two days
- Pain or discomfort in one or both eyes
- Blurred or double vision
- Sensitivity to light
- Sticky or pus-like discharge
- Swelling in or around the eyes
- Foreign body sensation that doesn’t go away
Early diagnosis and treatment can prevent complications and ensure a faster recovery.
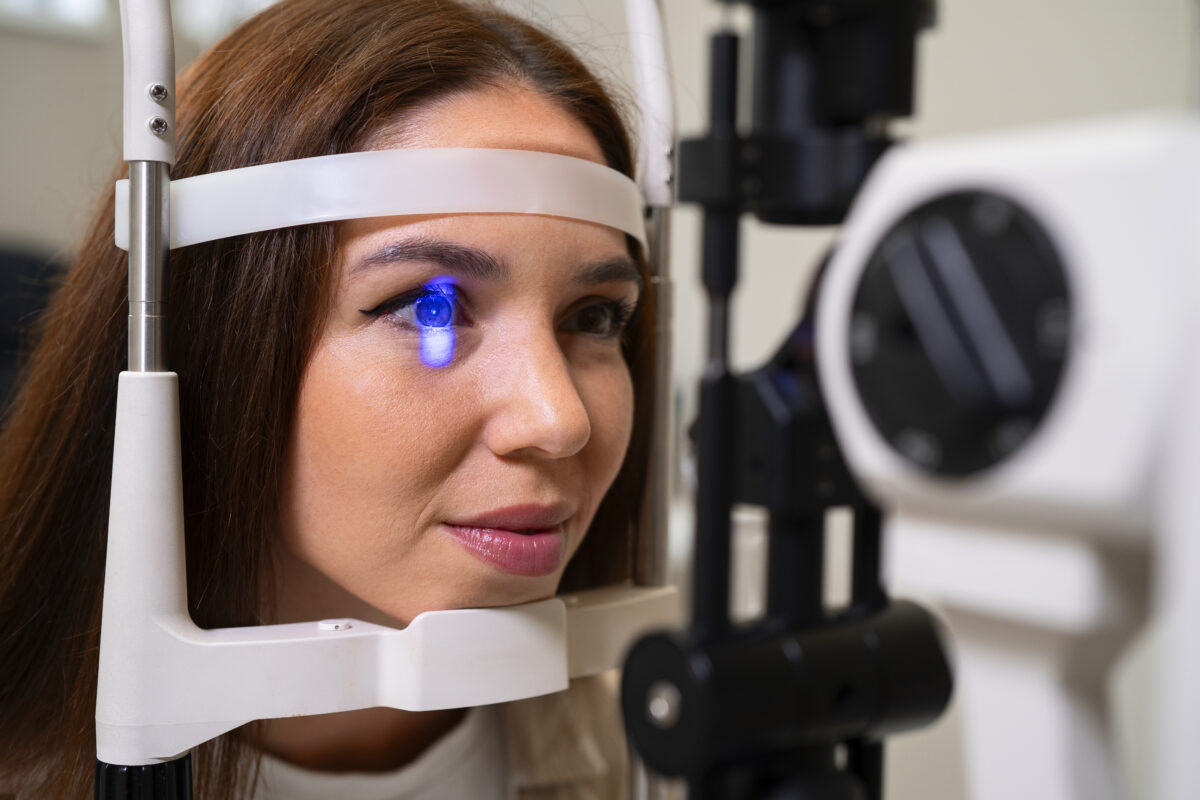
Role of Advanced Eye Clinics in Eye Vision Care
Monsoon-related eye problems may seem minor at first, but can escalate if ignored. That’s where expert care plays a vital role. Choosing a trusted eye care provider with experienced professionals and state-of-the-art facilities ensures you receive an accurate diagnosis and effective treatment.
Leading clinics offering eye vision treatment in Kerala combine advanced diagnostic technology, sterile environments, and personalized care to handle a range of seasonal and chronic eye conditions. From pediatric eye care to cataract and retina services, comprehensive solutions are available under one roof.
Protecting Your Vision This Monsoon: Key Takeaways
The monsoon may be a time for long drives, warm teas, and lush greenery — but it also requires extra care for your eyes. Maintaining eye hygiene, being cautious with contact lenses, and avoiding unnecessary exposure to rainwater can go a long way in preventing infections and irritation.
Remember, if your eyes are persistently itchy, red, or painful, don’t self-medicate. Instead, opt for expert care. Timely consultation with a reputed eye specialist treatment in Thrissur can help you protect your vision and keep your monsoon joyful and problem-free.